Understanding Adrenogenital Syndrome: Symptoms, Causes, Diagnosis, Treatment, and Coping Strategies
1. Introduction
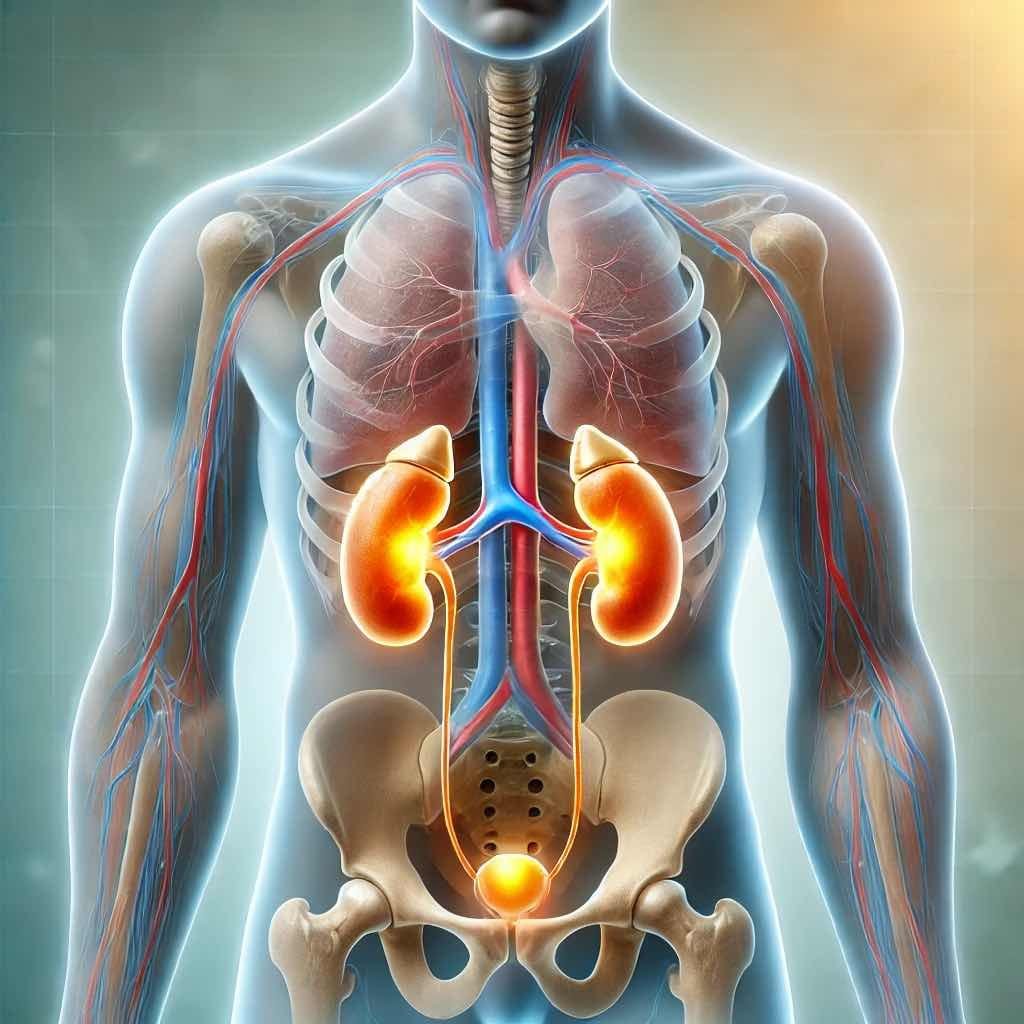
Adrenogenital syndrome, also known as congenital adrenal hyperplasia (CAH), is a genetic disorder affecting the adrenal gland’s ability to produce essential steroid hormones. These glands produce hormones essential for regulating metabolism, immune function, and stress response. In individuals with Adrenogenital Syndrome, the adrenal glands produce insufficient cortisol and often excessive androgens (male hormones) leading to various health issues. This condition typically results from a deficiency of 21-hydroxylase, an enzyme crucial for cortisol and aldosterone production. When the adrenal cortex fails to regulate hormone secretion properly, it leads to an excess of androgen hormones, causing symptoms such as abnormal secondary sex characteristics, adrenal hyperplasia symptoms, and, in severe cases, adrenal crisis.
In females, signs may include ambiguous genitalia at birth, menstrual irregularities, or excessive body hair due to high cortisol levels and hormonal imbalance. Adrenal testing, including cortisol blood tests and aldosterone hormone assessments, plays a critical role in diagnosing the disorder, with clinical guidelines recommending early detection for effective management.
2. Symptoms of Adrenogenital Syndrome
In females:
– Ambiguous genitalia in newborns
– Irregular menstrual periods
– Excessive facial and body hair
– Infertility
– Severe acne
– Male-pattern baldness
In males:
– Enlarged penis in male infants
– Early appearance of pubic hair
– Rapid growth during childhood
– Advanced bone age
– Shorter final height than expected
– Muscle development before the age of 10
In both sexes:
– Salt-wasting leading to dehydration, vomiting, and low blood pressure in severe cases
3. Causes of Adrenogenital Syndrome
Adrenogenital Syndrome is primarily caused by mutations in genes responsible for producing enzymes involved in cortisol and aldosterone synthesis. The most common form, 21-hydroxylase deficiency, leads to the build-up of androgens, causing the symptoms associated with the condition.
4. Diagnosis of Adrenogenital Syndrome
Diagnosing Adrenogenital Syndrome involves genetic testing, hormone level measurements, and imaging tests to assess the adrenal glands. Newborns are often screened for the condition as early detection and intervention are crucial for preventing salt-wasting crises and addressing ambiguous genitalia.
5. Treatment Options of Adrenogenital Syndrome
Treatment for adrenogenital syndrome focuses on restoring hormone balance through corticosteroid therapy to regulate cortisol levels and suppress excess androgen production. In cases of severe cortisol imbalance, patients may require long-term glucocorticoid treatment to prevent complications like Cushing’s syndrome or hypertension. Additionally, elevated cortisol treatment strategies aim to manage symptoms of high cortisol levels in females, such as facial puffiness (cortisol face) and metabolic disturbances. Clinical guides highlight the importance of regular endocrine system monitoring, as improper treatment can lead to conditions like primary hyperaldosteronism or pituitary gland deficiency. Ongoing research, as seen in PubMed articles and National Center for Biotechnology Information (NCBI) studies, continues to refine CAH treatment protocols, ensuring better outcomes for affected individuals.
– Medication: Cortisol replacement therapy is the cornerstone of treatment. Some individuals may also require aldosterone replacement.
– Lifestyle adjustments: Salt supplementation and regular medical follow-ups are essential to monitor hormone levels and prevent complications.
– Surgery: Genital reconstructive surgery may be considered for individuals with ambiguous genitalia.
6. Prevention Methods
As Adrenogenital Syndrome is a genetic condition, prevention primarily involves genetic counseling for families with a history of the disorder. Prenatal genetic testing can also help identify the condition early in pregnancy.
7. Living with Adrenogenital Syndrome
Coping strategies for individuals with Adrenogenital Syndrome involve adhering to medication schedules, maintaining a balanced diet, staying physically active, and seeking emotional support from healthcare professionals and support groups. Regular monitoring of hormone levels and adherence to treatment regimens are essential for managing the condition effectively.
8. Latest Research and Clinical Trials
Ongoing research focuses on optimizing hormone replacement therapies, improving fertility outcomes, and minimizing the long-term effects of Adrenogenital Syndrome. Clinical trials are also exploring new treatment modalities and potential gene therapies for individuals with specific gene mutations.
9. FAQs
Q1: Can Adrenogenital Syndrome be cured?
A1: Adrenogenital Syndrome is a lifelong condition, but with proper management, individuals can lead healthy lives.
Q2: Is Adrenogenital Syndrome fatal?
A2: With early diagnosis and appropriate treatment, the prognosis for individuals with Adrenogenital Syndrome is generally good.
Q3: Can individuals with Adrenogenital Syndrome have children?
A3: With proper medical management and fertility interventions if required, many individuals with Adrenogenital Syndrome can have children.
Q4: Are there any dietary restrictions for individuals with Adrenogenital Syndrome?
A4: Maintaining a balanced diet and monitoring salt intake are essential for individuals with Adrenogenital Syndrome. Consultation with a dietitian is recommended.
Q5: What are the long-term complications of Adrenogenital Syndrome?
A5: If left untreated, Adrenogenital Syndrome can lead to infertility, metabolic issues, and bone health concerns. Regular medical monitoring and adherence to treatment are crucial for minimizing long-term complications.
Q6: What are the common signs of hormonal imbalance?
A: Common symptoms include weight changes, fatigue, mood swings, irregular menstrual cycles, acne, insomnia, and low libido. The specific symptoms depend on which hormone is imbalanced.
Q7: How does hormonal imbalance affect cortisol levels?
A: Hormonal imbalance can lead to either high or low cortisol levels. High cortisol (linked to stress) can cause weight gain, anxiety, high blood pressure, and poor sleep, while low cortisol may result in fatigue and low blood pressure.
Q8: What role does the adrenal gland play in hormonal balance?
A: The adrenal glands produce key hormones like cortisol, aldosterone, and adrenaline. Dysfunction in these glands can lead to adrenal disorders such as Cushing’s syndrome or adrenal insufficiency.
Q9: Can a cortisol test help diagnose hormonal imbalance?
A: Yes, a cortisol blood, saliva, or urine test can measure cortisol levels and help diagnose adrenal gland disorders or stress-related hormonal imbalances.
Q10: What causes high cortisol levels?
A: Chronic stress, adrenal tumors, excessive caffeine intake, certain medications, and conditions like Cushing’s syndrome can lead to elevated cortisol levels.
Q11: How can I naturally regulate my cortisol levels?
A: Managing stress, getting enough sleep, following a balanced diet, reducing caffeine, and practicing relaxation techniques like meditation can help maintain healthy cortisol levels.
Q12: What is the link between hormonal imbalance and hypertension?
A: High cortisol and aldosterone levels can lead to increased blood pressure, contributing to hypertension. Adrenal gland disorders like primary hyperaldosteronism are a known cause of high blood pressure.
Q13: Can hormonal imbalance affect secondary sex characteristics?
A: Yes, imbalances in sex hormones like estrogen and testosterone can impact physical traits such as body hair growth, voice changes, muscle mass, and fat distribution.
Q14: Are there specific medical guidelines for treating hormonal imbalance?
A: Yes, clinical guidelines from organizations like the National Center for Biotechnology Information (NCBI) and PubMed provide recommendations for diagnosing and managing hormonal disorders.
Q15: When should I seek medical advice for a suspected hormonal imbalance?
A: If you experience persistent symptoms such as unexplained weight gain, severe fatigue, irregular menstrual cycles, extreme stress, or changes in blood pressure, consult a healthcare professional for proper diagnosis and treatment.
In conclusion, Adrenogenital Syndrome, though challenging, can be effectively managed with a multidisciplinary approach involving medication, lifestyle modifications, and regular medical follow-ups. Ongoing research offers hope for improved treatment strategies and better outcomes for individuals affected by this condition.
Related Diseases and Conditions
Adrenogenital Syndrome: एक विस्तृत जानकारी
1. परिचय
Adrenogenital Syndrome, जिसे कॉन्जेनिटल एड्रेनल हाइपरप्लेशिया (CAH) भी कहा जाता है, एक विकार है जो वृद्धि और लिंगानुपातिक विकास में बदलाव कर सकता है। यह विकार नाभिक ग्रंथियों के परिस्थितियों की वजह से होता है जो एड्रेनल ग्रंथियों द्वारा निर्मित हार्मोन कार्पा और एल्डोस्टेरोन की वृद्धि को बढ़ा देती है।
2. लक्षण
कुछ प्रमुख लक्षणों में शामिल हो सकते हैं: आबादी में वृद्धि, बालों का झड़ना, लिंग विकास में असामान्यता, महिलाओं में अंधवास्त्रक के कारण गर्भावस्था के समय संकेत, और बच्चों में असामान्य लिंग विकास।
3. कारण
एजेसी की विकृति: इस सिंड्रोम का मुख्य कारण एजेसी नामक एन्जाइम की विकृति होती है, जिसके कारण एड्रेनल ग्लैंड्स में असामान्य रूप से अधिक अंधवास्त्रक बनता है।
4. निदान
डॉक्टर एक परीक्षण के बाद और कुछ विशेष परीक्षण करने के बाद आपकी स्थिति को निदान करेंगे।
5. उपचार विकल्प
उपचार के विकल्प में शामिल हो सकते हैं: दवाइयाँ जो एड्रेनल ग्लैंड्स की स्थिति को संतुलित करने में मदद करती हैं, हार्मोन थेरेपी, और चिकित्सा जर्नलॉजी के नवीनतम उपकरणों का उपयोग।
6. रोकथाम के तरीके
एड्रेनोजेनिटल सिंड्रोम को रोकने के लिए जीवनशैली में बदलाव, नियमित चेकअप, और दवाओं का समय पर उपयोग किया जा सकता है।
7. Adrenogenital Syndrome के साथ जीना
संभावना है कि एड्रेनोजेनिटल सिंड्रोम वाले व्यक्ति को उपयुक्त चिकित्सा सलाह और सहायता की आवश्यकता हो सकती है।
8. नवीनतम शोध और नैदानिक परीक्षण
नवीनतम शोध और नैदानिक परीक्षण इस बीमारी के विशेष निदान और उपचार में मदद कर सकते हैं।
9. अक्सर पूछे जाने वाले प्रश्न
1. क्या एड्रेनोजेनिटल सिंड्रोम ठीक हो सकता है ?
एड्रेनोजेनिटल सिंड्रोम जीवन पर्यंत बीमारी है, लेकिन सही उपचार और नियमित चेकअप के माध्यम से इसका प्रबंधन किया जा सकता है।
2. क्या इस बीमारी का इलाज संभव है?
हां, एड्रेनोजेनिटल सिंड्रोम का उपयुक्त उपचार और प्रबंधन संभव है।
3. क्या यह बीमारी बच्चों में होती है?
हां, एड्रेनोजेनिटल सिंड्रोम बच्चों में हो सकती है।
4. क्या इस बीमारी का जीवनशैली पर प्रभाव होता है?
जी हां, यह बीमारी व्यक्ति की जीवनशैली पर प्रभाव डाल सकती है।
5. क्या इस बीमारी के लिए जीनेटिक टेस्ट मौजूद हैं?
हां, एड्रेनोजेनिटल सिंड्रोम का जीनेटिक टेस्ट मौजूद है।
10.डिस्क्लेमर
इस ब्लॉग में दी गई जानकारी केवल सूचनात्मक उद्देश्यों के लिए है और यह पेशेवर चिकित्सा सलाह, निदान, या उपचार का विकल्प नहीं है। किसी भी चिकित्सा स्थिति या उपचार के बारे में प्रश्नों के लिए हमेशा अपने चिकित्सक या अन्य योग्य स्वास्थ्य सेवा प्रदाता से परामर्श करें।इस ब्लॉग की सामग्री के कारण पेशेवर चिकित्सा सलाह की अनदेखी न करें या उसे प्राप्त करने में देरी न करें। यहां उल्लिखित उपचार सभी के लिए उपयुक्त नहीं हो सकते हैं और व्यक्तिगत परिस्थितियों के आधार पर जोखिम पैदा कर सकते हैं। किसी भी दवा या उपचार योजना को शुरू करने या बदलने से पहले हमेशा एक लाइसेंस प्राप्त स्वास्थ्य सेवा पेशेवर से परामर्श करें।
यहां तक कि यह ब्लॉग पेशेवर चिकित्सा सलाह की जगह नहीं है और न किसी भी चिकित्सा सलाह या उपचार के लिए उपयोग किया जाना चाहिए।
आपके स्वास्थ्य से जुड़े किसी भी परिस्थिति में, हमेशा अपने चिकित्सक या अन्य योग्य स्वास्थ्य सेवा प्रदाता से परामर्श करें।
Sources & Acknowledgments
This article is based on data from reputable sources, including:
- ClinicalTrials.gov – Providing the latest clinical trial information.
- OpenFDA – Offering reliable drug and medical device data.
We ensure all information is accurate, up-to-date, and aligned with expert-reviewed medical sources. Always consult a healthcare professional for medical advice.